Estimation of Fetal Weight and Age
Very small and very large babies have higher mortality and morbidity rates than infants of normal size. Because early detection of growth abnormalities may help prevent fetal demise and improve management of perinatal complications, monitoring of fetal growth is an important part of antepartum care.
Symphysis–fundal height (SFH)
Measurement of the symphysis-fundal height (SFH) is a common screening method used to estimate the gestational age and fetal growth after 24 weeks gestation. The SFH is measured using a tape placed over the mother's abdomen. The mother's bladder should be empty when the measurement is done. The distance from the top of the pubic bone (symphysis pubis) to the top of the pregnant uterus (fundus) is measured in centimeters (cm). The SFH in centimeters should be equal to the gestational age in weeks. A measurement discrepancy of more 3 cm is suggestive of a fetus with growth problems , an abnormal amniotic fluid level , a transverse lie, a twin pregnancy, or uterine fibroids [1,7].
The sensitivity of SFH measurement for detecting abnormal intrauterine growth was less than 35% in one study [2]. Roex A, et.al. found that the sensitivity of SFH measurement for detecting fetal growth abnormalities could be improved by serial plotting of the SFH on customized charts [3]. A Cochrane review concluded "There is insufficient evidence to determine whether SFH measurement is effective in detecting IUGR. We cannot therefore recommended any change of current practice. Further trials are needed." [4].
| Risk Factors for a Small for Gestational Age Neonate [5,20] | |
|---|---|
| Odds Ratio > 3 | Odds Ratio > 2 |
| Previous stillbirth | Maternal SGA |
| Antiphospholipid syndrome (APLS) | Chronic hypertension |
| Diabetes with vascular disease | PIH severe |
| Unexplained antepartum hemorrhage | Preeclampsia |
| Renal impairment | Smoking > 10 cigarettes/day |
| Low maternal weight gain | Low PAPP-A < 0.4 MoM |
| Paternal SGA | Threatened miscarriage |
| Low maternal weight gain | Elevated AFP > 2.0 MoM and hCG > 2.5 MoM |
| Cocaine use | Echogenic bowel in the fetus |
| Maternal age > 40 years | |
| Previous SGA baby | |
| Daily vigorous exercise | |
When there are factors that increase the risk for intrauterine growth restriction (IUGR) or the SFH is unreliable because of maternal obesity, twin pregnancy, polyhydramnios, or the presence of uterine leiomyomas (fibroids) ultrasonography may be a better screening modality for growth problems in the fetus..
Ultrasound estimate of gestational age and fetal growth
Prenatally the sonographically estimated fetal weight is used together with weight tables to evaluate fetal growth. Correct evaluation depends on the accuracy of the gestational age being used , the precision of the weight measurements , and using a weight curve that represents the population being studied.
Estimate of gestational age
The American College of Obstetricians and Gynecologists (ACOG) and the Society of Obstetricians and Gynaecologists of Canada recommend ultrasound measurement of the crown rump length (CRL) of the embryo or fetus as the most accurate method to establish or confirm gestational age [21,22]. The SOGC recommends the earliest ultrasound with a crown rump length equivalent to at least 7 weeks (or 10 mm) should be used to determine the gestational age. The SOGC also recommends "...either the best CRL or the average of several satisfactory measurements should be used." The ACOG recommends "The measurement used for dating should be the mean of three discrete CRL measurements when possible..." [21]. It is recommended that crown-rump length be used up to 84 mm, and other parameters be used for measurements > 84 mm [21, 22].
If the pregnancy is the result of in vitro fertilization, embryo age at transfer should be used to establish the estimated due date (EDD).
If the CRL > 84 mm the biparietal diameter (BPD) or head circumference (HC) is the best predictor of gestational age [25] . However, using multiple parameters is superior to using a single parameter to establish a gestational age in the second trimester [23]. Many regression equations are available using various combinations of parameters to estimate the gestational age. Some clinicians use the unweighted mean of the 4 most commonly used biometric parameters ( biparietal diameter (BPD), head circumference (HC), abdominal circumference (AC), and femur length (FL) ) to establish a gestational age [22]
Ultrasound estimate of fetal weight (EFW)
In practice, common equations for estimating fetal weight include the Hadlock formulas:
|
Shepard: Log10(weight) = -1.7492 + 0.166·BPD + 0.046·AC - 2.646·(AC·BPD)/1000 Hadlock 1: Log10(weight) = 1.304 + 0.05281·AC + 0.1938·FL - 0.004·AC·FL Hadlock 2: Log10(weight) = 1.335 - 0.0034·AC·FL + 0.0316·BPD + 0.0457·AC + 0.1623·FL Hadlock 3: Log10(weight) = 1.326 - 0.00326·AC·FL + 0.0107·HC + 0.0438·AC + 0.158·FL Hadlock 4: Log10(weight) = 1.3596 - 0.00386·AC·FL + 0.0064·HC + 0.00061·BPD·AC + 0.0424·AC + 0.174·FL |
Regardless of the formula used the accuracy of the sonographic estimate of the EFW is affected by supoptimal imaging and biological variation . In addition the accuracy of the sonographic estimate decreases with increasing birth weight [26,27] , and tends to be overestimated in pregnancies suspected of being large for gestational age (LGA) and underestimated in pregnancies with preterm premature rupture of membranes (PPROM) and suspected fetal growth restriction (FGR) [10].
Estimated Gestational Age and Fetal Weight Calculator
The calculator linked above uses Hadlock equations to estimate gestational age and fetal weight.
Evaluation of fetal growth
The average singleton fetus weighs about 80 grams (2.8 ounces) by the end of the first trimester and grows increasingly faster after 22 weeks to reach a maximum growth rate of almost 220 grams (7.8 ounces) per week by 35 weeks '. Growth then slows down and is about 185 grams (6.5 ounces) per week by 40 weeks [17]. Dichorionic twins grow at a similar rate to singletons until about 32 weeks .Thereafter dichorionic twins grow at about 188 grams per week until 37 weeks .Monochorionic twins growth rate growth begins to slow at 28 weeks and averages about 170 grams per week thereafter until 37 weeks [45]
Update: Twins—growth standards and fetal body composition
Twin-specific growth standards: Newer twin standards support that twins have growth patterns that differ from singletons, particularly later in gestation; using twin-specific references may reduce misclassification when assessing SGA/FGR in twin pregnancies [60,61].
Body composition (not just weight): Emerging evidence suggests twins and singletons differ in fetal soft-tissue/body composition measures (e.g., limb and abdominal soft tissue) from as early as 15 weeks, with differences increasing with gestational age [59]. These findings reinforce that EFW alone may not fully characterize “quality of growth,” particularly in twins.
See also: FMF twin growth charts (PDF) | ESPRiT twin biometry/outcomes (PMC) | Twins vs singletons body composition (PMC)
Estimated fetal weight percentile
After obtaining a reliable gestational age and best estimate of fetal weight, a growth chart or weight table may be used to assign an EFW growth percentile.
Singleton, Twin, and Preemie Growth Charts (click images to enlarge)
The Royal College of Obstetricians and Gynaecologists (RCOG) recommends that a fetal abdominal circumference (AC) or estimated fetal weight (EFW) less than 10th centile can be used to diagnose a small for gestational age (SGA) fetus. ACOG advises newborns whose birth weight is less than the 10th percentile for gestational age are considered small for gestational age (SGA) . Whereas a fetus with a weight that is less than the 10th percentile for its gestational age is considered to have fetal growth restriction (FGR), also known as intrauterine growth restriction (IUGR) [5, 7]. Large for gestational age (LGA) is generally used to describe a birth weight equal to or greater than the 90th percentile for a given gestational age [29]. However, there is not universal agreement on these definitions , and some have proposed the 15th and 97th percentiles as more optimal cut-offs to define SGA and LGA respectively [30].
For comparison , the table below shows the 10th and 90th percentiles for EFW from a Hadlock fetal growth curve and a neonatal birth weight curve using U.S. National Center for Health Statistics data from 2011 .
TABLE 1.
| Gestational Age Weeks |
EFW 10th Percentile | EFW 90th Percentile | |||
| Hadlock | Duryea | Hadlock | Duryea | ||
| 25 | 652 | 584 | 918 | 938 | |
| 26 | 758 | 637 | 1068 | 1080 | |
| 27 | 876 | 719 | 1234 | 1260 | |
| 28 | 1004 | 822 | 1416 | 1462 | |
| 29 | 1145 | 939 | 1613 | 1672 | |
| 30 | 1294 | 1068 | 1824 | 1883 | |
| 31 | 1453 | 1214 | 2049 | 2101 | |
| 32 | 1621 | 1380 | 2285 | 2331 | |
| 33 | 1794 | 1573 | 2530 | 2579 | |
| 34 | 1973 | 1793 | 2781 | 2846 | |
| 35 | 2154 | 2030 | 3036 | 3119 | |
| 36 | 2335 | 2270 | 3291 | 3380 | |
| 37 | 2513 | 2500 | 3543 | 3612 | |
| 38 | 2686 | 2706 | 3786 | 3799 | |
| 39 | 2851 | 2877 | 4019 | 3941 | |
| 40 | 3004 | 3005 | 4234 | 4057 | |
As can be seen from the above Table 1, the Hadlock derived fetal weights are higher than the data derived from the neonatal growth curve until about 37 weeks gestational age. Ott and more recently Solomon et. al., have suggested that IUGR is over-represented in premature deliveries and therefore the fetal growth standards may be more accurate than neonatal growth standards in evaluating the fetus at risk for IUGR [34,24]. Lackman F et al., have also advocated that "...intrauterine growth curves derived from ultrasonographically estimated fetal weight of continuing pregnancies are more appropriate than neonatal growth curves to discriminate fetuses and neonates at higher risk for adverse outcome ." [ 31]
The use of customized fetal growth charts has been proposed to improve the precision in evaluating fetal growth [5]. Table 2 shows data from the National Institute of Child Health and Human Development (NICHD) Fetal Growth Studies which demonstrates the differences in fetal growth between different races and ethnicities [51] . Not all agree that the use of custom growth charts improves prediction of perinatal mortality [6,7, 52,56-58]
TABLE 2
| Gestational Age (weeks) | EFW 10th Percentile (grams) | AC 10th Percentile (cm) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| White | Black | Hispanic | Asian | White | Black | Hispanic | Asian | ||
| 20 | 289 | 286 | 279 | 275 | 14.06 | 13.74 | 13.8 | 13.92 | |
| 21 | 349 | 342 | 336 | 331 | 15.2 | 14.81 | 14.9 | 15.02 | |
| 22 | 417 | 406 | 400 | 394 | 16.33 | 15.85 | 15.98 | 16.1 | |
| 23 | 495 | 478 | 473 | 466 | 17.44 | 16.88 | 17.04 | 17.15 | |
| 24 | 583 | 559 | 555 | 546 | 18.54 | 17.87 | 18.08 | 18.18 | |
| 25 | 682 | 650 | 646 | 637 | 19.61 | 18.85 | 19.1 | 19.19 | |
| 26 | 791 | 751 | 749 | 740 | 20.66 | 19.81 | 20.1 | 20.18 | |
| 27 | 912 | 863 | 862 | 853 | 21.7 | 20.76 | 21.1 | 21.15 | |
| 28 | 1045 | 985 | 987 | 978 | 22.72 | 21.72 | 22.09 | 22.12 | |
| 29 | 1188 | 1118 | 1123 | 1114 | 23.75 | 22.69 | 23.1 | 23.09 | |
| 30 | 1343 | 1262 | 1270 | 1260 | 24.78 | 23.68 | 24.12 | 24.08 | |
| 31 | 1509 | 1416 | 1428 | 1414 | 25.82 | 24.68 | 25.15 | 25.05 | |
| 32 | 1686 | 1579 | 1595 | 1574 | 26.84 | 25.68 | 26.18 | 26.02 | |
| 33 | 1869 | 1749 | 1769 | 1740 | 27.84 | 26.65 | 27.18 | 26.96 | |
| 34 | 2058 | 1923 | 1947 | 1911 | 28.81 | 27.58 | 28.14 | 27.87 | |
| 35 | 2247 | 2096 | 2125 | 2085 | 29.75 | 28.45 | 29.04 | 28.73 | |
| 36 | 2432 | 2264 | 2298 | 2262 | 30.63 | 29.27 | 29.87 | 29.54 | |
| 37 | 2609 | 2427 | 2463 | 2437 | 31.45 | 30.06 | 30.64 | 30.31 | |
| 38 | 2777 | 2587 | 2621 | 2604 | 32.19 | 30.83 | 31.36 | 31.06 | |
| 39 | 2934 | 2751 | 2774 | 2752 | 32.84 | 31.6 | 32.03 | 31.79 | |
| 40 | 3080 | 2922 | 2923 | 2873 | 33.38 | 32.4 | 32.67 | 32.52 | |
See also: World Health Organization Fetal Growth Calculator
The Small Fetus
Approximately 70% of infants born below the 10th percentile are not at risk for adverse outcomes. Differences in size are often constitutional (e.g., parental size, ethnicity, fetal sex). About 30% are truly growth restricted and are at increased risk for perinatal morbidity and mortality.
Fetal Growth Restriction (FGR) (also called Intrauterine Growth Restriction, IUGR)
SOGC and RCOG define FGR as an estimated weight < 10th percentile on ultrasound in a fetus that, because of a pathologic process, has not attained its biologically determined growth potential.
The Prospective Observational Trial to Optimize Pediatric Health in Intrauterine Growth Restriction (IUGR) (PORTO Study) found the presence of an abnormal umbilical artery Doppler ( pulsatility index >95th centile, absent end diastolic flow, or reversed end-diastolic flow) was significantly associated with adverse outcome*, in FGR fetuses irrespective of EFW percentile or abdominal circumference measurement. A sonographic EFW < 3rd percentile was consistently associated with adverse outcome ; all mortalities had EFW< 3rd centile. [8]
*Adverse perinatal outcome was defined as a composite of intraventricular hemorrhage, periventricular leukomalacia, hypoxic ischemic encephalopathy, necrotizing enterocolitis, bronchopulmonary dysplasia, sepsis, and death.
ACOG recommends "If the ultrasonographically estimated fetal weight is below the 10th percentile for gestational age, further evaluation should be considered, such as amniotic fluid assessment and Doppler blood flow studies of the umbilical artery. Because growth-restricted fetuses have a high incidence of structural and genetic abnormalities, an ultrasonographic examination of fetal anatomy also is recommended if not performed already." [7]
Twins
-
Birth weight discordance in twins refers to the difference in weight between two twins:
- Birth weight discordance = (larger twin weight − smaller twin weight) / larger twin weight × 100.
- See: Twin Birth Weight Discordance Calculator
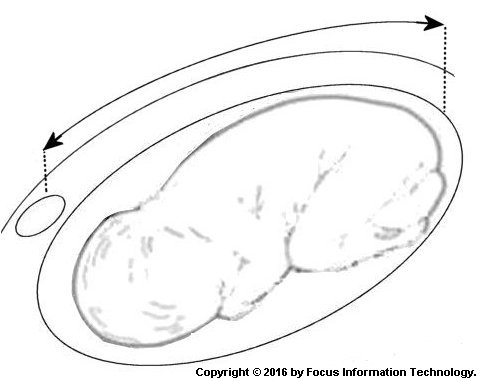
- Selective intrauterine growth restriction (sIUGR) is present when the fetal weight of one twin is below the 10th percentile [17] in one twin of a monochorionic twin pregnancy while the co-twin is of normal size . sIUGR affects 12 - 25 % of monochorionic (one placenta) twin pregnancies and is thought to be caused by unequal sharing of the placenta by the twins [9]
- Classification of sIUGR [9]:
- Type I (positive end-diastolic flow in the umbilical artery)
- Type II (AREDF) : persistently absent or reversed end-diastolic flow
- Type III (iAREDF). intermittent absent or reversed end-diastolic flow in the absence of fetal breathing.
Gratacós E, et. .al have suggested fetuses with sIUGR may be classified into three types based on one of three main umbilical artery Doppler waveform patterns, as defined by the characteristics of diastolic flow: positive, persistently absent/reversed or intermittently absent/reversed .
The Large Fetus
Large for gestational age (LGA) generally implies a birth weight equal to or greater than the 90th percentile for a given gestational age [29] .
Macrosomia "implies growth beyond a specific weight, usually usually 4,000 grams or 4,500 grams regardless of the gestational age" [29, 35, 36] , Boulet SL, et al have advocated dividing macrosomia into 3 grades based on the morbidity and mortality associated with birth weight ranges above 4000 grams [33]
- Grade 1: > 4000 g — increased risks of labor and newborn complications.
- Grade 2: > 4500 g — increased risk of neonatal morbidity.
- Grade 3: > 5000 g — increased risk of infant mortality.
Ye J and colleagues have suggested macrosomia be defined as a birth weight greater than 4300 grams (9 pounds 8 ounces) in Blacks and Hispanics or 4500 grams (9 pounds 15 ounces) in Whites regardless of gestational age. In addition a birth weight greater than the 97th percentile for a given gestational age, irrespective of race is reasonable to define macrosomia [32]
TABLE 3.
| Gestational Age Weeks |
EFW 90th Percentile (grams) | EFW 97th Percentile (grams) | |||||||
| White | Black | Hispanic | Asian | White | Black | Hispanic | Asian | ||
| 20 | 381 | 376 | 379 | 373 | 407 | 401 | 407 | 400 | |
| 21 | 460 | 451 | 456 | 447 | 491 | 481 | 489 | 480 | |
| 22 | 551 | 536 | 544 | 532 | 588 | 572 | 584 | 571 | |
| 23 | 654 | 633 | 643 | 628 | 698 | 676 | 691 | 674 | |
| 24 | 771 | 742 | 755 | 737 | 824 | 792 | 812 | 790 | |
| 25 | 903 | 864 | 882 | 859 | 964 | 923 | 948 | 921 | |
| 26 | 1050 | 1000 | 1023 | 997 | 1121 | 1069 | 1100 | 1069 | |
| 27 | 1212 | 1151 | 1180 | 1149 | 1295 | 1231 | 1270 | 1232 | |
| 28 | 1391 | 1317 | 1353 | 1318 | 1487 | 1409 | 1457 | 1413 | |
| 29 | 1587 | 1498 | 1543 | 1501 | 1697 | 1604 | 1662 | 1609 | |
| 30 | 1799 | 1695 | 1749 | 1698 | 1926 | 1816 | 1885 | 1821 | |
| 31 | 2029 | 1908 | 1971 | 1908 | 2174 | 2045 | 2126 | 2047 | |
| 32 | 2276 | 2135 | 2209 | 2129 | 2441 | 2290 | 2384 | 2284 | |
| 33 | 2537 | 2373 | 2460 | 2360 | 2724 | 2548 | 2657 | 2534 | |
| 34 | 2809 | 2619 | 2719 | 2600 | 3021 | 2816 | 2940 | 2795 | |
| 35 | 3088 | 2868 | 2983 | 2851 | 3326 | 3087 | 3229 | 3067 | |
| 36 | 3368 | 3115 | 3245 | 3111 | 3635 | 3356 | 3517 | 3352 | |
| 37 | 3645 | 3359 | 3502 | 3376 | 3942 | 3624 | 3802 | 3644 | |
| 38 | 3918 | 3605 | 3756 | 3637 | 4246 | 3896 | 4086 | 3933 | |
| 39 | 4186 | 3863 | 4011 | 3884 | 4548 | 4182 | 4372 | 4210 | |
| 40 | 4450 | 4142 | 4273 | 4105 | 4850 | 4494 | 4670 | 4462 | |
Hoopmann and colleagues compared 36 different weight formulas for the estimation of fetal weight for the prediction of macrosomia. They concluded that none of the 36 weight formulas reached a detection rate and false positive rate for fetuses >or=4,500 g that could lead to clinical recommendation [37]. Accuracy of the EFW is reported to be best when examinations are performed within 7 days before delivery [38]. One study found prenatal ultrasound diagnosis of prediction of birth weight to be no more accurate than maternal or clinical predictions of infant birth weight [39]. .
ACOG advises "An accurate diagnosis of macrosomia can be made only by weighing the newborn after delivery." [55]
Reviewed 3/31/2019
References
- Fetal Growth Disorders. In: Cunningham FG, ed. Williams Obstetrics. 22nd ed. McGraw-Hill; 2005:901.
- Sparks TN, et al. Fundal height: a useful screening tool for fetal growth? J Matern Fetal Neonatal Med. 2011;24(5):708–712. doi:10.3109/14767058.2010.516285. PMID: 20849205
- Roex A, et al. Serial plotting on customised fundal height charts results in doubling of the antenatal detection of SGA fetuses in nulliparous women. Aust N Z J Obstet Gynaecol. 2012;52(1):78–82. doi:10.1111/j.1479-828X.2011.01408.x. PMID: 22309365
- Robert Peter J, et al. Symphysial fundal height (SFH) measurement in pregnancy for detecting abnormal fetal growth. Cochrane Database Syst Rev. 2015;(9):CD008136. doi:10.1002/14651858.CD008136.pub3.
- RCOG Green-top Guideline No. 31. The investigation and management of the small-for-gestational-age fetus. 2013/2014. PDF
- Hutcheon JA, et al. BJOG. 2008;115(11):1397–1404. doi:10.1111/j.1471-0528.2008.01870.x. PMID: 18823489
- ACOG Practice Bulletin No. 134. Fetal growth restriction. Obstet Gynecol. 2013;121:1122–1133.
- Unterscheider J, et al. Optimizing the definition of intrauterine growth restriction: the multicenter prospective PORTO Study. Am J Obstet Gynecol. 2013;208(4):290.e1–290.e6. doi:10.1016/j.ajog.2013.02.007. PMID: 23531326
- Gratacós E, et al. Classification system for selective IUGR in monochorionic pregnancies by UA Doppler. Ultrasound Obstet Gynecol. 2007;30(1):28–34. PMID: 17542039
- Ben-Haroush A, et al. Accuracy of sonographically estimated fetal weight in 840 women with pregnancy complications. Ultrasound Obstet Gynecol. 2004;23(2):172–176. PMID: 14770399
- Hadlock FP, et al. Fetal crown-rump length and menstrual age (5–18 weeks). Radiology. 1992;182(2):501–505. PMID: 1732970
- Hadlock FP, et al. Estimating fetal age: computer-assisted analysis of multiple parameters. Radiology. 1984;152(2):497–501. PMID: 6739822
- Shepard MJ, et al. Evaluation of two equations for predicting fetal weight by ultrasound. Am J Obstet Gynecol. 1982;142:47.
- Hadlock FP, et al. Sonographic estimation of fetal age and weight. Radiol Clin North Am. 1990;28(1):39–50. PMID: 2404304
- Hadlock FP, et al. Estimation of fetal weight using head, body, and femur measurements. Am J Obstet Gynecol. 1985;151(3):333–337. PMID: 3881966
- Doubilet PM, Benson CB. Sonographic evaluation of IUGR. AJR Am J Roentgenol. 1995;164(3):709–717. PMID: 7863900
- Hadlock FP, et al. In utero analysis of fetal growth: a sonographic weight standard. Radiology. 1991;181(1):129–133. PMID: 1887021
- Ott WJ. The diagnosis of altered fetal growth. Obstet Gynecol Clin North Am. 1988;15(2):237–263. PMID: 3067166
- Duryea EL, et al. A revised birth weight reference for the United States. Obstet Gynecol. 2014;124(1):16–22. doi:10.1097/AOG.0000000000000345. PMID: 24901276
- Odibo AO, et al. Marker screening thresholds associated with IUGR. Am J Perinatol. 2006;23(6):363–367. PMID: 16841275
- ACOG Committee Opinion No. 611. Method for estimating due date. Obstet Gynecol. 2014;124(4):863–866. PMID: 25244460
- SOGC Guideline No. 303. Determination of gestational age by ultrasound. J Obstet Gynaecol Can. 2014;36(2):171–181.
- Hill LM, et al. Composite assessment of gestational age. Am J Obstet Gynecol. 1992;166(2):551–555. PMID: 1536228
- Salomon LJ, et al. EFW reference range at 20–36 weeks and comparison with birth-weight reference. Ultrasound Obstet Gynecol. 2007;29(5):550–555. PMID: 17444561
- Reddy UM, et al. Fetal imaging workshop executive summary. J Ultrasound Med. 2014;33(5):745–757. PMID: 24764329
- Ben-Haroush A, et al. EFW in diabetic pregnancies and suspected macrosomia. J Perinat Med. 2004;32(2):113–121. PMID: 15085885
- Mongelli M, Benzie R. Ultrasound diagnosis of fetal macrosomia: comparison of models. Ultrasound Obstet Gynecol. 2005;26(5):500–503. PMID: 16180258
- Alsulyman OM, et al. Intrapartum US EFW in diabetic pregnancies. Am J Obstet Gynecol. 1997;177:503–506. PMID: 9322614
- Breathnach FM, et al. Definition of intertwin birth weight discordance. Obstet Gynecol. 2011;118(1):94–103. PMID: 21691168
- Ananth CV, et al. Birth weight discordancy and adverse outcomes among twin gestations. Am J Obstet Gynecol. 2003;188:954–960. PMID: 12712093
- Buck Louis GM, et al. Racial/ethnic standards for fetal growth: NICHD Fetal Growth Studies. Am J Obstet Gynecol. 2015;213(4):449.e1–449.e41. PMID: 26410205
- Carberry AE. Customized vs population-based charts and neonatal morbidity. Am J Epidemiol. 2013;178:1301–1308. PMID: 23966560
- Bukowski R, et al. Fetal growth and risk of stillbirth. PLoS Med. 2014;11(4):e1001633. PMID: 24755550
- Francis JH, et al. Perinatal mortality by birthweight centile. Aust N Z J Obstet Gynaecol. 2014. PMID: 24731210
- ACOG Practice Bulletin No. 173. Fetal macrosomia. Obstet Gynecol. 2016;128:e195–e209.
- Milner J, Arezina J. Accuracy of ultrasound EFW vs birth weight: systematic review. Ultrasound. 2018;26(1):32–41. PMID: 29456581
- Monier I, et al. Hadlock vs INTERGROWTH EFW formulas in a preterm population. Am J Obstet Gynecol. 2018;219(5):476.e1–476.e12. PMID: 30118693
- Blue NR, et al. Hadlock vs NICHD racial/ethnic standard for predicting morbidity/SGA. Am J Obstet Gynecol. 2018;219(5):474.e1–474.e12. PMID: 30118689
- Gleason JL, Lee W, Chen Z, Wagner KA, He D, Grobman WA, Newman RB, Sherman S, Gore-Langton R, Chien E, Goncalves L, Grantz KL. Fetal Body Composition in Twins and Singletons. JAMA Pediatr. 2025 Jun 1;179(6):630-638. doi: 10.1001/jamapediatrics.2025.0116. PMID: 40193121; PMCID: PMC11976649.
- Wright D, Wright A, Chaveeva P, Molina FS, Akolekar R, Nicolaides KH. Fetal Medicine Foundation charts for fetal growth in twins. Ultrasound Obstet Gynecol. doi: 10.1002/uog.27514. DOI; FMF PDF.
- Dicker P, Daly S, Conroy RM, et al. Fetal biometry reference ranges derived from prospective twin population and evaluation of adverse perinatal outcome. Ultrasound Obstet Gynecol. 2025;65(4):436-446. doi: 10.1002/uog.29190. PMID: 40014646; PMCID: PMC11961106.